
 health
health 
[ad_1]

When Dr. Tiffany M. Osborn received her COVID-19 vaccination shortly after vaccines became available in late 2020, she felt hopeful about the pandemic’s trajectory. A year later, she’s sad and frustrated to see so many COVID patients in the ICU.
Matt Miller / Washington University School of Medicine
hide caption
toggle caption
Matt Miller / Washington University School of Medicine

When Dr. Tiffany M. Osborn received her COVID-19 vaccination shortly after vaccines became available in late 2020, she felt hopeful about the pandemic’s trajectory. A year later, she’s sad and frustrated to see so many COVID patients in the ICU.
Matt Miller / Washington University School of Medicine
The latest surge in COVID-19 cases is testing the endurance of intensive care workers at Barnes-Jewish Hospital in St. Louis.
“You feel like, ‘What am I doing here?’ ” says Dr. Nguyet Nguyen, a pulmonary critical care specialist at the hospital and assistant professor of medicine at Washington University in St. Louis. “I’m working as hard as I can and still all of these people are dying.”
“We’re tired,” says Dr. Tiffany Osborn, a professor of surgery and emergency medicine. “We see so much needless suffering.”
Both doctors say unvaccinated people make up the vast majority of COVID-19 patients in the ICU. Neither doctor expected to be caring for so many desperately ill patients nearly a year after vaccines became widely available.
The toll on ICU workers has increased steadily, despite advances in both preventing and treating COVID-19.
From fear to fatigue
“In the early days, we were all very scared because we had no idea what this was,” Nguyen says.
“We didn’t know how to prevent it, and we didn’t know how to treat it,” Osborn says, “and there were a lot of concerns that many of us had about, can we bring this home to our family?”
So Osborn moved into an RV parked in her driveway. She accepted that, but struggled with the burden of watching so many of her patients die.
Often, the best Osborn could do was make sure a dying patient’s family got to say goodbye — and even that was only over the phone. One of those calls she helped facilitate from the ICU still haunts her.
“As I turned to leave, I hear this voice come over the phone, this small voice that says, ‘I love you, grandpa.’ And all I could do is close the door behind me as I left,” she says. “It’s a very helpless feeling.”

Caregivers working with COVID-19 patients in a Barnes-Jewish Hospital intensive care unit write a message of love and support on the glass door facing a patient’s room.
Matt Miller / Washington University School of Medicine
hide caption
toggle caption
Matt Miller / Washington University School of Medicine
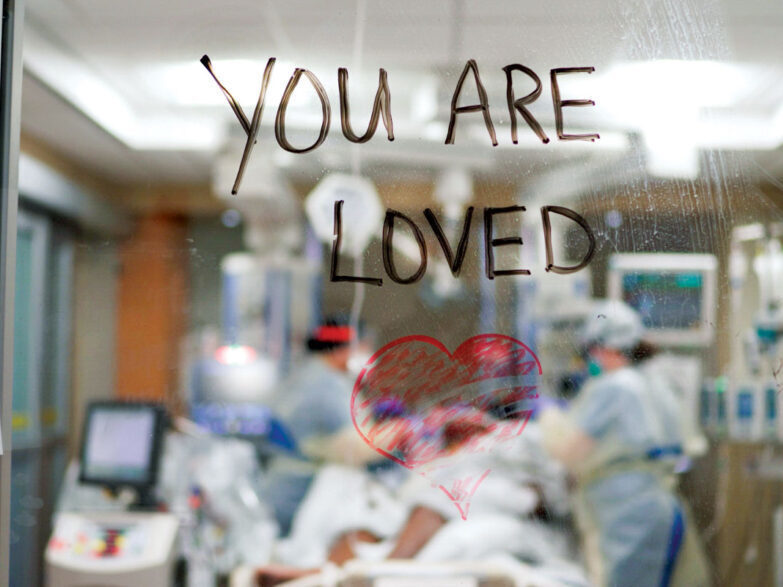
Caregivers working with COVID-19 patients in a Barnes-Jewish Hospital intensive care unit write a message of love and support on the glass door facing a patient’s room.
Matt Miller / Washington University School of Medicine
When vaccines began to arrive in late 2020, though, Osborn saw reason for hope.
“When you got that vaccine it was like you could feel the pressure coming off of your shoulders,” she says.
Health care workers could finally protect themselves with something other than masks and gloves PPE. And it looked like widespread vaccination would reduce the flow of critically ill patients from a torrent to a trickle.
Fast forward a year, though, and that still hasn’t happened.
“Most of the people who come to the ICU are still unvaccinated, and they did not have to be where they ended up being,” Nguyen says. “So it’s very frustrating for us to deal with that on a day to day basis.”
The fatigue and frustration may be most acute for intensive care nurses and respiratory therapists, who provide most of the hands-on care in the ICU, Nguyen says. In St. Louis, many have retired early or switched jobs.
Nguyen thinks she understands why.
“We’re used to dealing with death, but not at the level that we saw with COVID,” she says. “And [we saw] people who were so young, and people who — they didn’t have to die.”
ICU teams are still having to place otherwise healthy, young COVID patients on the last-ditch life-support machines known as ECMO (extracorporeal membrane oxygenation), Osborn says.
“We have capacity for about 12 ECMO machines,” she says. “During our last surge, half of them were [being used for] pregnant women.”
And most of those pregnant women were unvaccinated.
Nguyen wishes that people who still haven’t been vaccinated knew more about what happens to COVID patients in an ICU.
“I don’t think that people understand that for a certain unlucky population, COVID is going to kill you,” she says. “And it’s going to kill you a lot faster than you think.”
When COVID patients arrive in the ICU, Nguyen says, she often explains that they need to make decisions about their care right away because within a few hours, many ICU patients are no longer able to speak or think clearly.
BRACING FOR OMICRON
For many weary health care professionals, Nguyen says, each new wave of COVID-19 has been like a punch in the face. “We felt like we were over the peak of Delta and then Omicron comes rolling in and just knocks everybody down again.”
ICU teams are better prepared now than they were at the beginning of the pandemic. They’ve learned what works to keep COVID patients alive, and there are new drugs arriving that promise to reduce the severity of infections.
Even so, the nation needs to focus on prevention rather than counting on treatment, Osborn says.
“This holiday season is really all about those interactions with the people we care so much about,” she says. “You don’t want it to have to be from a hospital bed with me holding up a telephone so you can talk with your family.”
[ad_2]
Source